March 07, 2000 --
Ng Min Li
Physiotherapist

Urinary incontinence is the involuntary passage of urine thus creating a hygienic and social problem. It can range from an occasional leakage of urine to a total loss of control. Incontinence is a symptom, not a disease. Many people with incontinence are too embarrassed to seek help and they often become withdrawn socially. This is very unfortunate as most cases of incontinence can be treated and controlled, if not cured completely.
Incidence
Incontinence can occur at all ages, but the risk increases with age. It is rare in children. Incontinence in children may be associated with urinary tract infections, spinal cord injuries and abnormalities of the nervous system that result in abnormal bladder control. Incontinence occurs more frequently in the elderly; it is estimated that 50 percent of the elderly in nursing homes are affected while about 20-30 percent of those living at home suffer from incontinence. In the non-elderly group, incontinence is an embarrassing problem for women in the childbearing years. Incontinence affects both men and women, but it is more common in women than in men.
The urinary system
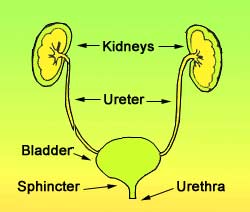
The urinary system consists of two kidneys, two ureters, a bladder, and a urethra. There is also a circular muscle surrounding the urethra called the sphincter that has a role to play in incontinence.
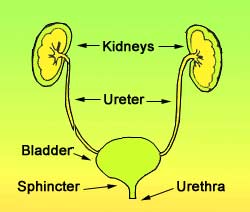 Urine produced in the kidneys is passed via the ureters to the bladder where it is stored until the bladder is emptied. The bladder is a muscular bag that can store up to 300-500ml of urine. The narrow, internal opening of the urethra within the bladder is called the bladder neck. In this region, the bladder's bundled muscular fibres help the sphincter muscles to close the urethra.
Urine produced in the kidneys is passed via the ureters to the bladder where it is stored until the bladder is emptied. The bladder is a muscular bag that can store up to 300-500ml of urine. The narrow, internal opening of the urethra within the bladder is called the bladder neck. In this region, the bladder's bundled muscular fibres help the sphincter muscles to close the urethra.
The urethra is the outlet from the bladder. It passes through the pelvic floor muscles in front of the vagina (birth canal connected to the uterus/womb). These muscles, like the sphincter muscles, act like a control valve around the urethra. They tighten when you cough or exercise and relax when urine is passed.
When the bladder is filled to about 200ml, a signal is sent to the brain to indicate an urge to pass urine. When you pass urine, the sphincter muscles and pelvic floor muscles relax while the bladder contracts to squeeze out the urine. Most people empty their bladder 4-6 times a day passing 200-300ml of urine each time.
Types of incontinence
There are several types of incontinence:
- Stress incontinence.
Stress incontinence is the leakage of urine when the pressure in the abdomen increases (e.g. during exercise, coughing, sneezing, laughing, lifting heavy objects and straining when passing motion). Stress incontinence is not due to emotional stress, but physical stress that puts pressure on the bladder. It results from stretching and weakening of the pelvic floor muscles that occurs during childbirth, surgery or weight gain. Without adequate support from these muscles, the pelvic organs (bladder, bowel and uterus) may slip down from their normal positions (prolapse) and push the bladder neck out of its correct position causing sphincter incompetence. Often, menopause worsens the problem due to the reduced levels of oestrogen (female hormone). It is the most common type of incontinence in women and can usually be cured.
- Urge incontinence.
Urge incontinence is the involuntary passage of urine due to an inability to control the urge and hold the urine long enough to reach a toilet. Urge incontinence results from an overactive or oversensitive bladder that contracts suddenly regardless of the amount of urine it holds. Urge incontinence is commonly caused by bladder infection, nerve damage, alcohol consumption or some medications. Besides being common in menopausal women, it also tends to occur in people with Parkinson's disease, stroke, multiple sclerosis, dementia and diabetes.
- Overflow incontinence.
Overflow incontinence is the leakage of small amounts of urine from a bladder that is always full. There is a constant feeling of fullness of the bladder that results in frequent and long visits to the toilet. However, despite much effort, there is an inability to empty the bladder completely and only a weak, dribbling stream of urine is produced. Overflow incontinence can result from a blocked urethra (e.g. an enlarged prostate compressing on the urethra in men) or a loss of normal bladder contractions in some people with diabetes.
- Functional incontinence.
Functional incontinence occurs in many older people who have normal urinary control, but who have difficulty reaching a toilet in time because of arthritis or other disabling disorders.
- Mixed Incontinence.
As the name implies, mixed incontinence is a combination of two or more types of incontinence.
Treatment and management of incontinence
In order to effectively treat and manage incontinence, the doctor must perform a detailed medical examination. This involves taking a detailed history of one's health and related problems as well as a physical examination that focuses on the urinary and reproductive systems. Treatment is individualised and may include any of the following measures.
- Behavioural techniques. Pelvic floor exercises and bladder training are commonly used for stress and urge incontinence. Besides having no adverse effects, their efficacy has also been demonstrated in many studies. Hence, behavioural techniques form the first line of treatment.
- Medication. A number of medications can be used to treat incontinence. Certain medications prevent the bladder from over contracting and are suitable for the treatment of urge incontinence. Some improve the bladder sphincter function, and are thus particularly useful for stress incontinence. Oestrogen may also be used to restore elasticity and tension in the urethra and vagina, which improves symptoms. However, these drugs may cause side effects such as dryness of mouth, drowsiness, eye problems, and retention of urine; therefore, they must be used carefully under a doctor's supervision.
- Surgery. In some cases, surgery provides a possible solution. This invariable relates to a structural problem such as an abnormally positioned bladder or blockage due to an enlarge prostate. Sometimes, injections of collagen or fat are given on each side of the urethra to provide bulk support for a weak bladder neck.
Sometimes, incontinence cannot be cured but it can be managed in several ways.
- Incontinence pads. Absorbent pads, kept in place with special elastic briefs are available for moderate incontinence. For mild incontinence, a sanitary pad may be adequate. Adult diapers are convenient for the bed-ridden.
- Self-catheterisation. A flexible tube known as a catheter can be inserted into the urethra to collect the urine in a container. However, catheterisation can increase the risk of urinary tract infections. In men, an alternative to the indwelling catheter is an external collecting device. This is fitted over the penis and connected to a drainage bag.
Prevention
-
Do not keep your urine for long periods (e.g. 5 to 6 hours) before emptying your bladder. This causes the bladder to become over-stretched and weakened, leading to overflow incontinence.
-
Exercise your pelvic floor muscles regularly, especially during pregnancy and post delivery.
-
Before coughing, sneezing or other exertion, brace the pelvic floor muscles.
-
Keep healthy and fit. Maintain a healthy diet and exercise regularly to avoid putting on excessive weight.
Pelvic floor muscles
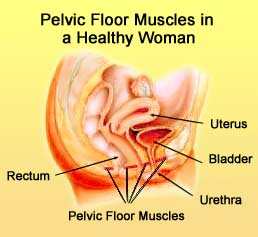 The pelvic floor muscles form a hammock at the bottom of the pelvis, and support the bladder, bowel and uterus. These muscles help control the outlets from these organs, and are especially important in urinary control. Like other muscles of the body, these muscles can be strengthened through proper exercise.
The pelvic floor muscles form a hammock at the bottom of the pelvis, and support the bladder, bowel and uterus. These muscles help control the outlets from these organs, and are especially important in urinary control. Like other muscles of the body, these muscles can be strengthened through proper exercise.
Exercising the pelvic
floor muscles
To perform the exercises properly, you need to find the correct muscles. Seek the help of your doctor or physiotherapist or nurse who can help you locate the right muscles as well as monitor your progress. Below is a simple exercise programme:
-
Think of your pelvic floor muscles and pull them up as hard as you can as though you are preventing the flow of urine or the passing of wind. Do not squeeze your buttock or tummy muscles. Then, let go. Do 5 or 6 repetitions in a row. ("Fast Repetitions").
-
After a short time, the muscles will feel stronger. Then begin "Slow Holds". Tighten the muscles and hold the contraction before letting go slowly. Do not hold your breath. Gradually increase the hold time to 6 seconds. Initially, do 5 of these, with a short rest between each hold, and then gradually increase the repetitions to 10.
-
If your muscles are weak, it is better to start the exercise in a position where least pressure is on them:
(i) lying on your back with your knees bent and feet flat on the bed, or
(ii)lying on you back with your legs straight and slightly apart.
Once you have mastered the exercise, you can perform these exercises in various positions (sitting or standing) or even when you are walking.
-
To get the correct feel of the pelvic floor muscles working, try to stop the flow of urine in mid-stream. Concentrate on how this feels. DO NOT do this every time you visit the toilet as it can cause urinary reflux leading to urinary tract infection.
-
Success does not happen overnight. You need to work on these muscles daily for several months and you will notice an improvement in your urinary control. Aim to do at least 100 to 150 "Slow Holds" daily.
Exercise aids
Biofeedback or electrical stimulation are sometimes used in training the pelvic floor muscles. A biofeedback monitor can help you to determine whether you are contracting the right muscles as well as the strength of your contractions. Brief doses of electrical stimulation can facilitate the contraction of these muscles, especially in the initial stage of the training, in the individual with very weak pelvic floor muscles. Electrodes are temporarily placed in the vagina or rectum to painlessly stimulate nearby muscles.
Remember: You are not alone. Seek medical help. Be optimistic. Be persistent in your exercise and you will reap the rewards!
References:
- Burgio KL, Locher JL, Goode PS, et al (1998): "Behavioral vs. drug treatment for urge urinary incontinence in older women" Journal of American Medical Association 280:1995-2000
- Laycock J, Green RJ (1988): "Interferential therapy in the treatment of incontinence" Physiotherapy 74:161-168
- Nasr SZ, Ouslander JG (1998): "Urinary incontinence in the elderly: causes and treatment options" Drugs and Aging 12:349-360
Date reviewed: May 20, 2005

 Urine produced in the kidneys is passed via the ureters to the bladder where it is stored until the bladder is emptied. The bladder is a muscular bag that can store up to 300-500ml of urine. The narrow, internal opening of the urethra within the bladder is called the bladder neck. In this region, the bladder's bundled muscular fibres help the sphincter muscles to close the urethra.
Urine produced in the kidneys is passed via the ureters to the bladder where it is stored until the bladder is emptied. The bladder is a muscular bag that can store up to 300-500ml of urine. The narrow, internal opening of the urethra within the bladder is called the bladder neck. In this region, the bladder's bundled muscular fibres help the sphincter muscles to close the urethra. 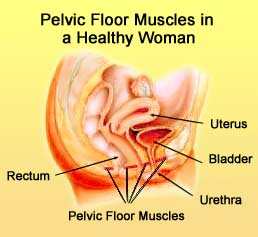 The pelvic floor muscles form a hammock at the bottom of the pelvis, and support the bladder, bowel and uterus. These muscles help control the outlets from these organs, and are especially important in urinary control. Like other muscles of the body, these muscles can be strengthened through proper exercise.
The pelvic floor muscles form a hammock at the bottom of the pelvis, and support the bladder, bowel and uterus. These muscles help control the outlets from these organs, and are especially important in urinary control. Like other muscles of the body, these muscles can be strengthened through proper exercise.